

An additional risk of pericarditis is the development of constrictive pathophysiology. After pericardiotomy, pericarditis is more common, with a likely incidence between 10% and 25% (13,14). Early pericarditis after ST-segment elevation MI has also decreased (approximately 4%), although it is more common in patients who present after at least 6 h of symptoms (14%) and in patients with percutaneous coronary intervention failure (23%) (12). In the current era of early reperfusion for acute MI, late pericarditis (Dressler’s syndrome) is uncommon (<0.5%) (11,12). In patients who have had an initial recurrence, additional recurrence occurs in 25% to 50% (9,10).Ī separate question relates to the risk of developing a first episode of pericarditis after cardiac injury. In the United States and Western Europe, most episodes of pericarditis (80% to 90%) are so-called “idiopathic” and are often presumed to be post-viral (5).ĭeath in patients hospitalized for acute pericarditis is uncommon (1%), and mortality is most often not related to pericarditis (6) 1% to 2% of patients will have pericardial tamponade during the first acute attack.Īfter an episode of acute pericarditis, the probability of developing incessant pericarditis or a first recurrence within 18 months is generally 15% to 30% (7,8).
Trivial pericardial effusion free#
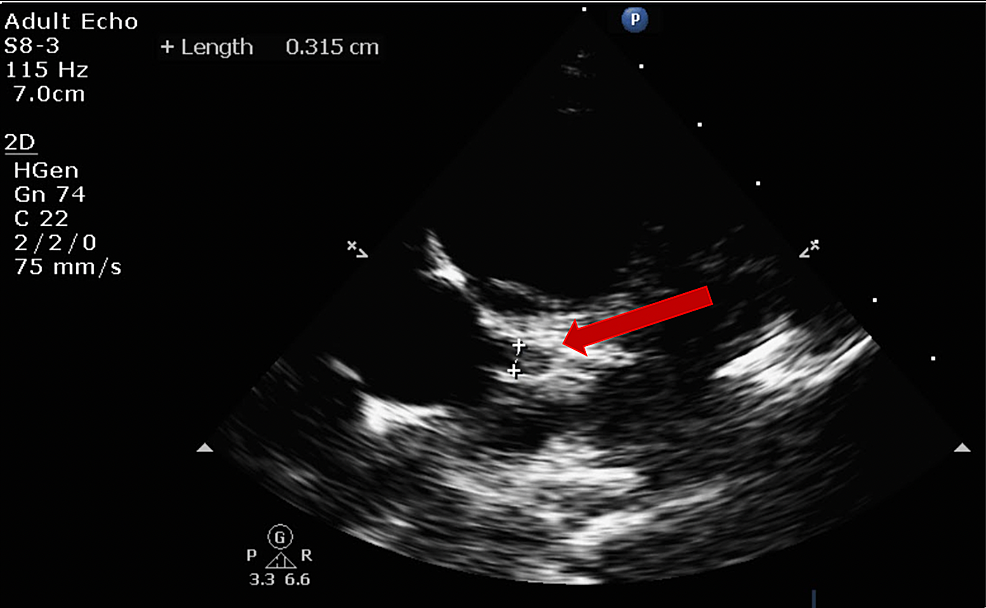
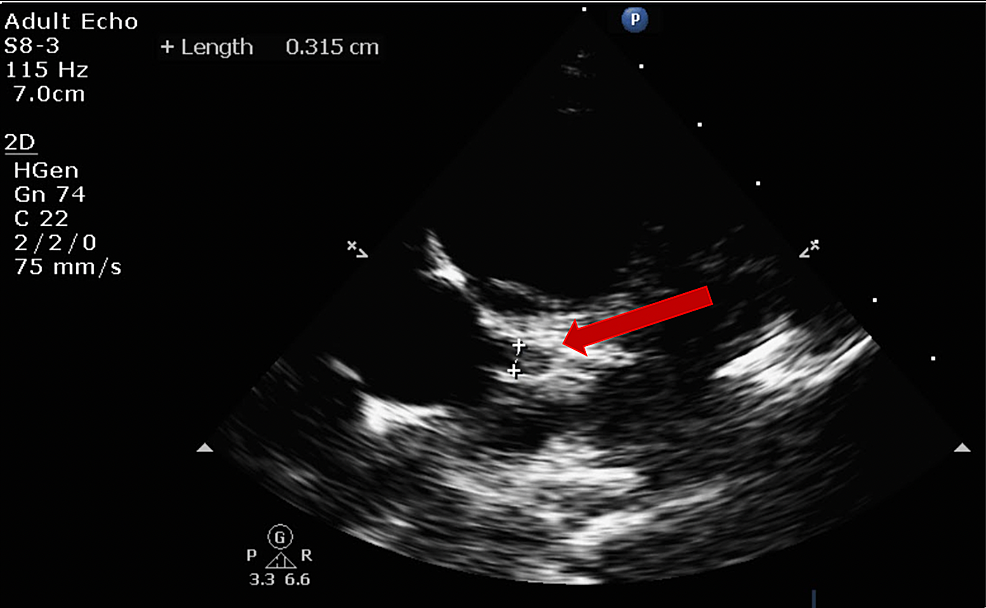
recurrent (a relapse occurring after a period in which the patient is free of symptoms for at least 4 to 6 weeks) (2),. chronic (presence of symptoms for >3 months),. incessant (pericarditis that persists for more than 4 to 6 weeks),. In practice diagnosis is made when chest pain is associated with either ECG changes (50-60% of cases), pericardial effusion (60%), or a friction rub (30%) (2-4).Ĭomplicated pericarditis is defined as one of the following clinical entities: Summary Clinical entities and identifying the patient at risk for complicated pericarditisĭiagnosis of pericarditis requires at least 2 of the following criteria: precordial chest pain that is worse with inspiration and when supine, characteristic ST-segment elevation and PR deviation on ECG, a pericardial friction rub, and a pericardial effusion that is more than trivial (1). What are the established treatments for pericarditis, and what are the emerging therapies for patients with complicated disease. What is the pathological progression of pericarditis, and how is autoinflammatory pericarditis distinct from autoimmune pericarditis. Which patients with complicated pericarditis benefit from multimodality imaging. 
 Which patients are at risk for complicated disease after acute pericarditis,. Many of these patients experience a debilitating chronic disease, and are referred in this review to as having complicated pericarditis. Although most patients with acute pericarditis will have resolution, some will develop incessant, recurrent, chronic, or constrictive pericarditis. Rarely a review paper is covered in this section, but this review was so interesting that we made an exception. KleinĬommented by: Antonio Brucato and Silvia Maestroni, Internal Medicine, Ospedale Papa Giovanni XXIII Bergamo, Italy Background Cremer, Arnav Kumar, Apostolos Kontzias, Carmela D.
Which patients are at risk for complicated disease after acute pericarditis,. Many of these patients experience a debilitating chronic disease, and are referred in this review to as having complicated pericarditis. Although most patients with acute pericarditis will have resolution, some will develop incessant, recurrent, chronic, or constrictive pericarditis. Rarely a review paper is covered in this section, but this review was so interesting that we made an exception. KleinĬommented by: Antonio Brucato and Silvia Maestroni, Internal Medicine, Ospedale Papa Giovanni XXIII Bergamo, Italy Background Cremer, Arnav Kumar, Apostolos Kontzias, Carmela D.






 0 kommentar(er)
0 kommentar(er)
